Middle Ear Infection
Ear infections are among the most common illnesses of early childhood. Three out of four children have had at least one ear infection by age 3, according to the National Institute on Deafness and Other Communication Disorders.
The medical term for middle ear infections is Otitis media. Otitis refers to inflammation of the ear, and media means middle.
Although ear infections worry parents and make children uncomfortable, take heart. Most ear infections clear up on their own within a few days, and most children stop having ear infections once they reach school age.

Symptoms
Ear infections can be hard to detect, especially if your child is too young to say, "My ear hurts." Knowing what to look for can help. Children with ear infections may:
• Tug or pull at their ears
• Cry more than usual
• Have trouble sleeping
• Fail to respond to sounds
• Be unusually irritable
• Develop a fever
• Develop fluid that drains from the ears
• Have headaches

Causes
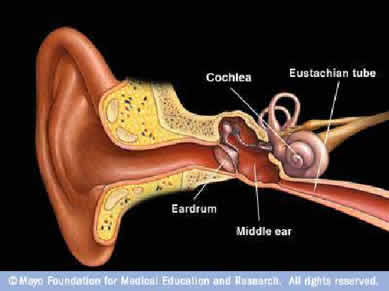
Ear infections usually start with a viral infection, such as a cold. The middle ear becomes inflamed from the infection, and fluid builds up behind the eardrum.
Ear infections also can be associated with dysfunction or swelling within the Eustachian tubes - the narrow passageways that connect the middle ear to the nose. Normally these tubes equalize pressure inside and outside the ear. But a child's Eustachian tubes are narrower and shorter than those of an adult. This makes it easier for fluid to get trapped in the middle ear when the Eustachian tubes dysfunction or become blocked during a cold.
Another factor in ear infections is swelling of the adenoids. These are tissues located in the upper throat near the Eustachian tubes. Adenoids contain lymphocytes - cells that normally fight infection. But sometimes the adenoids themselves get infected or enlarged, blocking the Eustachian tubes. Infection in the adenoids can also spread to the Eustachian tubes.
In addition, children don't have fully developed immune systems. So it's easier for them to develop many illnesses, including colds and ear infections.
Risk Factors
Age
Children between ages 6 and 18 months are the most susceptible to ear infections, although ear infections are common from ages 4 months to 4 years.
Group Child Care
Children cared for in group settings are more likely to get colds and ear infections than are children who stay home.
Reduced Air Quality
Children with exposure to tobacco smoke or higher levels of air pollution are at higher risk of ear infections.
Family history
Your child's risk of ear infections increases if another member of the family has had such infections.
Race
American Indians and Eskimos from Alaska or Canada tend to have more ear infections than do caucasians.
Feeding Position
Babies who drink from a bottle while lying down tend to have more ear infections than do babies who are held upright during feedings.
Season
Ear infections are most common during the fall and winter.

When to Seek Medical Advice
Ear infections aren't usually an emergency, but they can make your child uncomfortable. If your child's signs and symptoms last longer than a day, call your child's doctor. In children younger than age 2, watch for sleeplessness and irritability after an upper respiratory infection, such as a cold. Call your child's doctor if you see a discharge of blood or pus from the ear. This could indicate a ruptured eardrum. If your child has already been diagnosed with an ear infection, call the doctor if your child's signs and symptoms don't improve or they get worse.
Screening and Diagnosis
There are two main types of ear infections:
Acute Otitis Media (AOM).
In AOM, parts of the ear are infected and swollen, and fluid and mucus are trapped inside the ear.
Otitis Media with Effusion (OME).
Effusion refers to fluid. In OME, fluid stays in the ear after the infection has cleared up. The presence of fluid increases the risk of a new infection.Ear infections are diagnosed based on your child's medical history and a physical exam. During the exam, the doctor will look for inflammation in the middle ear with a lighted instrument known as an otoscope.
A related instrument is the pneumatic Otoscopes, which allows the doctor to gently puff air on the eardrum. Normally this causes the eardrum to move. Any fluid in the middle ear will prevent that movement.
Sometimes additional tests for ear infections are recommended, especially if your child has had fluid in the middle ear for some time:
Tympanometry.
This test also measures eardrum movement. A soft plug is inserted into the opening of the ear. The plug includes a device that changes air pressure inside the ear.Acoustic Reflectometry.
During this test, the doctor uses a hand-held instrument to project sounds of varying frequencies into the ear. How the sounds are reflected indicates differences between empty space and fluid.
Complications
Many ear infections clear on their own with no complications. However, long-lasting or recurrent infections can lead to:
Short-term Hearing Loss
Fluid buildup can temporarily affect your child's hearing. That's because it's harder for the eardrum and the tiny bones in the middle ear to send sound vibrations through fluid. The average hearing loss is 25 decibels - about the same as putting plugs in your child's ears.
Long-term Hearing Loss
Usually the fluid disappears on its own in a few weeks. But sometimes it remains in the middle ear for months, which can damage the eardrum and bones in the middle ear. Persistent middle ear fluid was once thought to contribute to speech or developmental delays, but researchers now say this isn't true.
Ruptured Eardrum
During ear infections, fluid and pus may press against the eardrum. This can be painful. Rarely, the pressure ruptures the eardrum. If this happens, you may see a discharge of pus and blood from your child's ear. This can be alarming. But the rupture actually relieves your child's pain, and in most cases the eardrum heals on its own. If the eardrum ruptures repeatedly and doesn't heal, surgical repair may be needed.
Untreated ear infections also can lead to a type of sinusitis known as mastoiditis, which affects the mastoid bone of the skull. Rarely, infections can move from the ear to other parts of the head, including the brain.
Treatment Options
Ear infections can be treated various ways. What's best for your child depends on many factors, including your child's age, medical history and the type of ear infection.
Read more...
Middle Ear Infection (Otitis media) Treatment Options